Pseudarthrosis (Nonunion): A Complete Guide to Causes, Symptoms, and Treatment
Key points
- Persistent or Worsening Pain: A deep, aching pain at the site that may be constant or flare up with activity. In spinal pseudarthrosis, this can be neck or back pain.
- Radiating Pain: Pain that travels from the spine into the shoulders, arms, or legs (radicular pain).
- Instability: A feeling that the bone or joint is not stable or secure.
- Neurological Symptoms: Numbness, tingling, or weakness if the false joint is compressing nearby nerves.
- Reduced Mobility: Difficulty moving the affected limb or area of the spine.
- Clicking or Grinding Sounds: A noticeable sound or sensation with movement.
Pseudarthrosis, also known as nonunion, is a medical term for a bone fracture that fails to heal correctly. Instead of the broken pieces knitting back together into a solid bone, a fibrous, unstable connection forms, creating a "false joint" (from the Greek pseudo- meaning false, and arthrosis meaning joint). This condition can lead to persistent pain, instability, and a significant impact on quality of life, particularly when it occurs after spinal fusion surgery.
This comprehensive guide synthesizes information from leading medical journals, health institutions, and patient surveys to provide a complete overview of pseudarthrosis, from its underlying causes to the latest treatment options.
What is Pseudarthrosis?
Normally, after a bone breaks, the body initiates a complex healing process to bridge the gap and form new, solid bone. When this process is interrupted or fails, a nonunion or pseudarthrosis occurs. This condition is a significant complication following fractures and is particularly challenging when it happens after a spinal fusion—a surgical procedure intended to permanently connect two or more vertebrae to eliminate motion and relieve pain.
According to research published in the Journal of the American Academy of Orthopaedic Surgeons, pseudarthrosis is the result of a failed spinal fusion attempt and can manifest months or even years after the initial surgery [1]. While it can happen to any bone, it is most common in long bones like the tibia (shin bone) and in the spine.
!X-ray showing pseudarthrosis of the tibia
X-ray image demonstrating a clear nonunion (pseudarthrosis) in the tibia.
Source: Radiopaedia.org, rID: 15479
Symptoms: Recognizing the Signs of a Failed Fusion
While some individuals with pseudarthrosis may be asymptomatic, many experience noticeable symptoms. The most common sign is persistent pain at the fracture or surgery site long after it should have healed.
Key symptoms include:
- Persistent or Worsening Pain: A deep, aching pain at the site that may be constant or flare up with activity. In spinal pseudarthrosis, this can be neck or back pain.
- Radiating Pain: Pain that travels from the spine into the shoulders, arms, or legs (radicular pain).
- Instability: A feeling that the bone or joint is not stable or secure.
- Neurological Symptoms: Numbness, tingling, or weakness if the false joint is compressing nearby nerves.
- Reduced Mobility: Difficulty moving the affected limb or area of the spine.
- Clicking or Grinding Sounds: A noticeable sound or sensation with movement.
Interestingly, a study noted that around 30% of people with radiographically confirmed pseudarthrosis report no symptoms at all [2].
Uncovering the Causes and Risk Factors
The failure of a bone to heal is often a multifactorial problem, involving a combination of biological, mechanical, and lifestyle-related issues. Understanding these risk factors is crucial for both prevention and treatment.
Patient-Related and Lifestyle Factors
Certain personal health conditions and habits can significantly interfere with the body's healing capacity.
- Smoking: This is one of the most significant risk factors. Nicotine constricts blood vessels, reducing blood flow and the delivery of oxygen and nutrients essential for bone healing. It also inhibits the function of osteoblasts, the cells responsible for forming new bone [3].
- Age: Older individuals may have slower healing processes and reduced bone quality.
- Medical Conditions: Diseases like diabetes, osteoporosis, severe anemia, and metabolic disorders can compromise bone health and repair [4].
- Obesity: Excess weight places additional stress on healing bones, particularly in the spine, which can hinder fusion.
- Poor Nutrition: Deficiencies in crucial nutrients like calcium, vitamin D, and protein can prevent the body from building strong bone tissue.
- Medications: Long-term use of steroids and non-steroidal anti-inflammatory drugs (NSAIDs) can interfere with bone healing.
Surgical and Mechanical Factors
The nature of the injury and the surgical procedure itself play a vital role.
- Inadequate Immobilization: If the fractured bone or fusion site is not held perfectly still, the constant micromotion can prevent bone cells from bridging the gap.
- Poor Blood Supply: Certain bones have a naturally limited blood supply. Severe trauma that damages surrounding blood vessels can also lead to nonunion.
- Infection: A bacterial infection at the surgical site can overwhelm the body's healing response.
- Surgical Technique: The success of a fusion can depend on the surgeon's technique, including proper preparation of the bone surfaces and secure placement of hardware (screws and rods).
- Multi-level Fusions: Fusing multiple vertebrae at once increases the mechanical stress and biological demand, raising the risk of pseudarthrosis at one or more levels.
How Pseudarthrosis is Diagnosed
Diagnosing pseudarthrosis involves a combination of a thorough clinical evaluation and advanced imaging. A doctor will first discuss your symptoms and medical history, followed by a physical examination.
The definitive diagnosis is typically made with imaging studies:
- X-rays: Standard X-rays, particularly flexion-extension views (where you bend forward and backward), can reveal a lack of bone bridging the fracture gap or show motion between vertebrae that were supposed to be fused.
- Computed Tomography (CT) Scans: CT scans provide a much more detailed, three-dimensional view of the bone. Thin-cut CT scans are considered the gold standard for assessing whether a solid fusion has formed and can identify even small gaps in the bone [1].
- Magnetic Resonance Imaging (MRI): An MRI may be used to evaluate the surrounding soft tissues, such as nerves and discs, to rule out other causes of pain.
Dr. Alpesh Patel discusses stable pseudarthrosis in athletes. Source: Cervical Spine Research Society on YouTube.
Congenital vs. Acquired Pseudarthrosis
It's important to distinguish between pseudarthrosis that develops after an injury or surgery (acquired) and a rare form that is present at birth (congenital).
| Feature | Congenital Pseudarthrosis | Acquired Post-Surgical Nonunion |
|---|---|---|
| Onset | Present at birth or develops in early childhood. | Occurs after a fracture or surgery in a previously normal bone. |
| Common Location | Most often affects the tibia (shin bone). | Can occur in any bone, but common after spinal fusion. |
| Underlying Cause | A developmental abnormality where bone tissue is inherently dysplastic (abnormal). Often associated with neurofibromatosis type I (NF-I). | Failure of the normal healing process due to various risk factors (e.g., smoking, infection, instability). |
| Bone Quality | The affected bone segment is weak and has poor healing potential. | The bone is typically healthy before the fracture. |
| Treatment Focus | Complex reconstructive surgery to excise abnormal tissue and achieve a stable union. | Addressing the specific cause of nonunion and stimulating healing. |
| Prognosis | Challenging, with a high risk of refracture and persistent nonunion, sometimes requiring multiple surgeries. | Generally favorable with appropriate treatment, leading to high rates of successful union. |
A 2025 study in the Journal of Orthopaedic Surgery and Research highlights the complexities of treating congenital pseudarthrosis of the tibia (CPT), noting that even necessary corrective osteotomies (bone cuts) are controversial due to healing concerns [5].
A Spectrum of Treatment Options
Treatment for pseudarthrosis is tailored to the individual, depending on the location of the nonunion, the severity of symptoms, and the patient's overall health.
Non-Surgical Management
For patients who are asymptomatic or poor surgical candidates, conservative treatment may be the first choice.
- Bone Stimulators: These external devices use low-level ultrasonic or pulsed electromagnetic waves to encourage bone growth at the nonunion site.
- Bracing: A custom brace can be used to immobilize the area, reducing motion and pain while giving the bone another chance to heal.
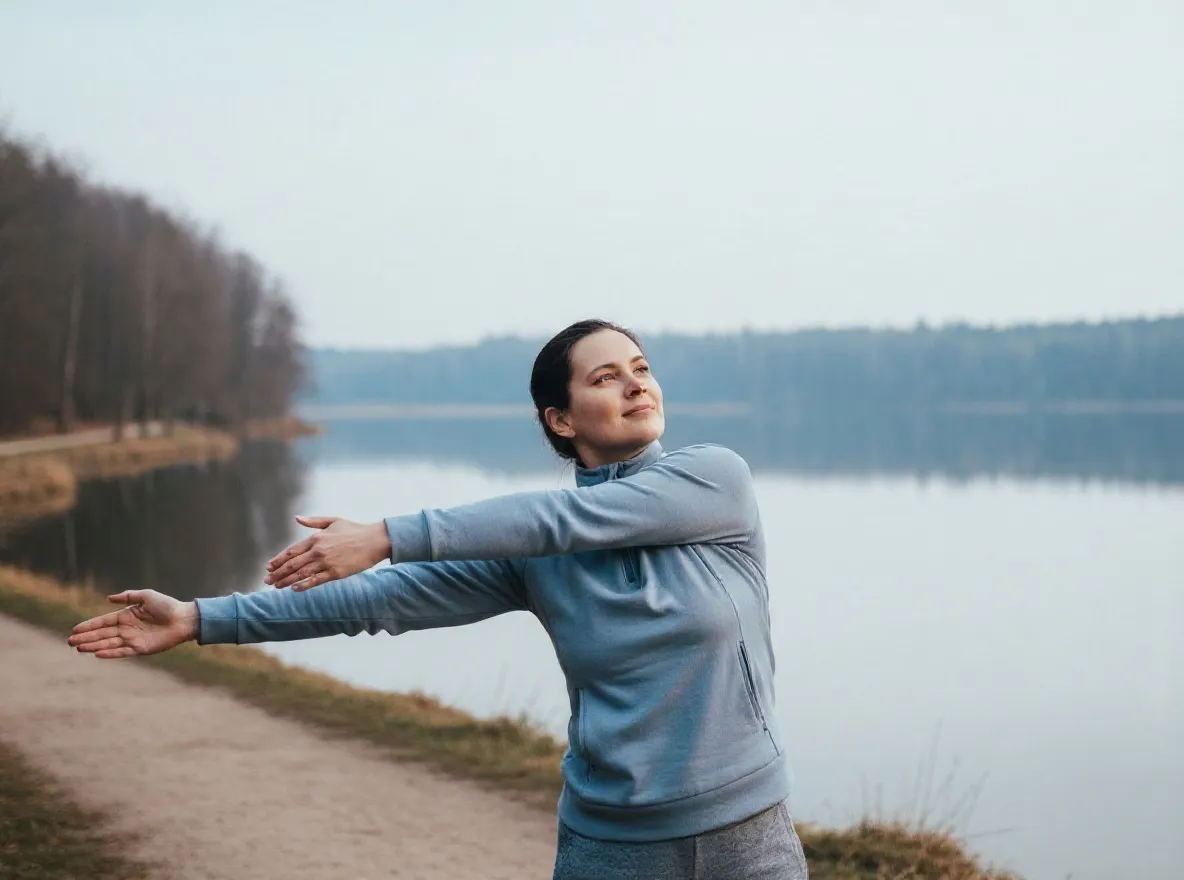
- Physical Therapy: Strengthening the muscles around the affected area can improve stability and function.
- Lifestyle Modifications: Quitting smoking, optimizing nutrition, and managing underlying conditions like diabetes are essential steps.
Surgical Intervention
When conservative treatments fail or symptoms are severe, surgery is often necessary. The goal of surgery is to establish stability and stimulate a robust biological healing response.
- Revision Surgery with Bone Grafting: This is the most common approach. The surgeon removes any failed hardware, excises the fibrous tissue from the "false joint," and prepares the bone ends to create a fresh surface for healing. A bone graft—either an autograft (bone taken from the patient's own body, often the pelvis) or an allograft (donor bone)—is packed into the gap to provide a scaffold and cells that promote new bone formation.
- Improved Fixation: New, more rigid hardware such as plates, screws, or rods are used to provide absolute stability.
- Biologics: In some cases, substances like Bone Morphogenetic Proteins (BMPs) may be used to powerfully stimulate bone growth.
- Electrical Stimulation: Studies have found that electrical stimulation devices, sometimes implanted internally, can significantly increase fusion rates after spinal surgery [6].
!Surgical fixation of a nonunion fracture
Surgical repair of a femoral nonunion using a plate and screws to provide stability.
Source: Wikimedia Commons, user Bone_and_joint
Prognosis and Life After Treatment
The outlook for patients with pseudarthrosis has improved with modern surgical techniques. With appropriate treatment, success rates for achieving a solid fusion can be as high as 80-90%.
However, the journey can be challenging. Revision surgery is often more complex than the initial procedure. Even after a successful fusion, some patients may experience persistent symptoms. The long-term impact on quality of life can be significant, particularly concerning mental health. Chronic pain and disability can lead to depression and anxiety, which may not fully resolve even after the physical issue is corrected.
A comprehensive approach that addresses both the physical and psychological aspects of the condition is crucial for achieving the best possible long-term outcome. If you are experiencing persistent pain after a fracture or fusion surgery, it is essential to consult with an orthopedic surgeon or spine specialist for a thorough evaluation.
References
- Raizman NM, O'Brien JR, Poehling-Monaghan KL, Yu WD. Pseudarthrosis of the spine. J Am Acad Orthop Surg. 2009 Aug;17(8):494-503. https://pubmed.ncbi.nlm.nih.gov/19652031/
- Leven D, Cho SK. Pseudarthrosis of the Cervical Spine: Risk Factors, Diagnosis and Management. Asian Spine J. 2016 Aug;10(4):776-86. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4995265/
- Cuellar Spine. Pseudarthrosis After Fusion Treatment & Symptoms. https://cuellarspine.com/insights/pseudarthrosis-after-fusion/
- MedicalNewsToday. Pseudarthrosis: Definition, symptoms, and treatments. https://www.medicalnewstoday.com/articles/pseudoarthrosis
- Liu, Y., Zhu, G., Liao, S. et al. Does an osteotomy performed in congenital pseudarthrosis of the tibia accompanied by tibial angular deformity heal?. J Orthop Surg Res 20, 397 (2025). https://josr-online.biomedcentral.com/articles/10.1186/s13018-025-05806-z
- Marquez-Lara A, D'Agostino R, Medda S, Ricciardi L, Ramhmdani S. Electrical stimulation therapy in spinal fusion: a cross-sectional analysis of indications and outcomes. J Neurosurg Spine. 2020 Jan 1;32(1):106-112. https://thejns.org/spine/view/journals/j-neurosurg-spine/32/1/article-p106.xml
Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for any health concerns or before making any decisions related to your health or treatment.
About the author
Samuel Jones, MD, is a board-certified orthopedic surgeon specializing in joint replacement and orthopedic trauma. He is a team physician for a professional sports team and practices at a renowned orthopedic institute in Georgia.