
What Vitamins Help With Sciatic Nerve Pain?
Discover which vitamins, like B12 and D, can support nerve health and potentially alleviate sciatic nerve pain as part of a holistic treatment plan.

Discover which vitamins, like B12 and D, can support nerve health and potentially alleviate sciatic nerve pain as part of a holistic treatment plan.

Discover the best stretches for a bulging disk in your neck and back. This guide offers safe, effective exercises for pain relief.

Explore the complete guide to neck surgery, including types like ACDF and disc replacement, reasons, recovery, risks, and FAQs.

Explore the causes, symptoms, and treatment for disc desiccation. Learn if it's serious, if it can be reversed, and why it might not always cause pain.

Explore the causes, symptoms, and comprehensive treatment options for disc desiccation. Learn about rehydration, surgery, and how lifestyle affects your spine.

Experiencing sharp back pain when you cough? Learn the common causes, from muscle strain to herniated discs, and discover effective treatments and prevention tips.

Understand levoscoliosis, a left-curving spine. Learn about its symptoms, causes, why it's a 'red flag,' and effective non-surgical and surgical treatments.

Tired of hip pain from sitting? Discover common causes like bursitis, tight hip flexors, and sciatica. Find expert-backed tips for relief and prevention.

Experiencing an ache in the back of your ribs? Learn the common musculoskeletal and internal causes, when to see a doctor, and how to find effective relief.

Explore desiccated disc, a common spine condition. Learn about its causes, symptoms, stages, diagnosis, and the latest treatment options from experts.

Experiencing knee pain with no obvious injury? Discover the surprising link between sciatica and knee pain, including symptoms, causes, and effective treatments.

Explore the critical differences between paraplegia and quadriplegia, including causes, symptoms, functionality, and the long-term outlook for each condition.
The human spine is a marvel of engineering, a complex structure providing central support that allows us to stand, bend, walk, and run. However, its intricacy also makes it susceptible to injury and degenerative conditions. In fact, an estimated eight in ten people will experience significant back pain at some point in their lives.
This guide serves as a comprehensive resource for understanding your back and spine, recognizing common problems, and navigating the vast landscape of modern medical care—from conservative therapies to advanced surgical interventions.
Your spine, or backbone, is not a single bone but a column of 33 individual bones called vertebrae, stacked one upon another. This column is grouped into four main regions:
Between each vertebra lie intervertebral discs—gel-like cushions that act as shock absorbers and allow for flexibility. The entire structure encases and protects the spinal cord, a critical bundle of nerves that transmits signals between your brain and the rest of your body.
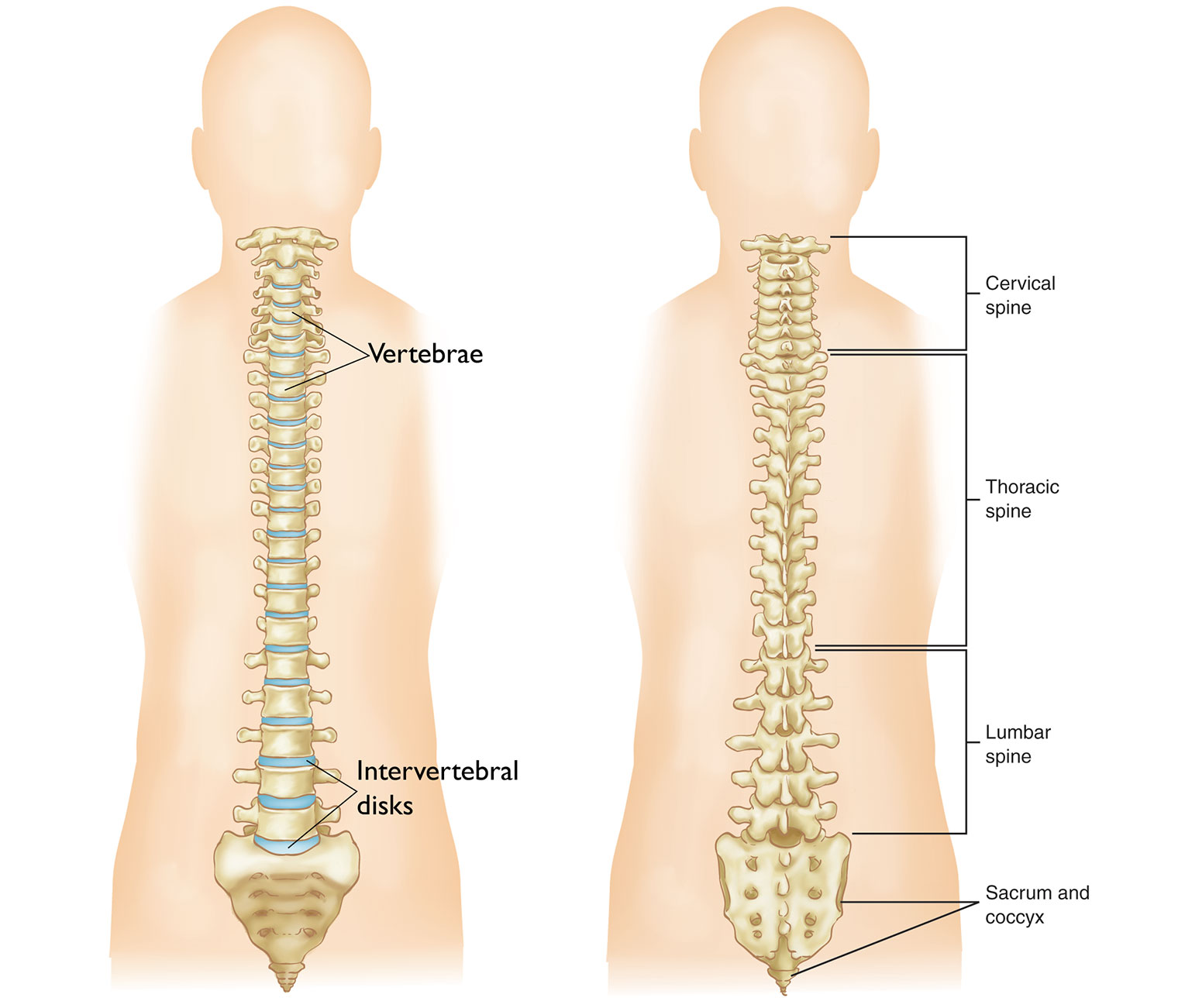 Image Source: OrthoInfo - American Academy of Orthopaedic Surgeons
Image Source: OrthoInfo - American Academy of Orthopaedic Surgeons
Pain and dysfunction arise when any of these components are compromised. Understanding the symptoms and underlying conditions is the first step toward effective treatment.
According to experts at UT Southwestern Medical Center, you should seek medical advice if you experience:
Spine specialists at centers like Texas Orthopedics and St. David's HealthCare regularly treat a wide range of conditions, including:
| Condition | Description |
|---|---|
| Herniated Disc | The soft center of a spinal disc pushes through its tough exterior, often pressing on a nerve. |
| Degenerative Disc Disease | The natural breakdown of spinal discs due to age, leading to pain and reduced flexibility. |
| Spinal Stenosis | A narrowing of the spinal canal, which can put pressure on the spinal cord and nerves. |
| Scoliosis & Kyphosis | Abnormal sideways (scoliosis) or forward (kyphosis) curvature of the spine. |
| Spondylolisthesis | A condition where one vertebra slips forward over the one below it. |
| Sciatica | Pain affecting the back, hip, and outer side of the leg, caused by compression of a spinal nerve root. |
| Facet Joint Syndrome | Arthritis-like condition of the joints connecting the vertebrae, causing pain and stiffness. |
When you're in pain, knowing which specialist to see can be confusing. Modern spine care is a collaborative field, and your treatment may involve several experts.
A physiatrist, or physical medicine and rehabilitation (PM&R) physician, specializes in diagnosing and treating nerve, muscle, and bone conditions without surgery. They are often the best starting point for back pain, as they can perform diagnostic tests, manage your pain with non-invasive treatments, and coordinate your care with other specialists like physical therapists.
If surgery is being considered, both orthopedic surgeons and neurosurgeons are qualified to operate on the spine. The best choice often depends on the specific condition.
Many leading spine centers, like the HSS Spine department, have both types of surgeons on staff who collaborate to provide comprehensive care. The most critical factor is finding a surgeon who is fellowship-trained in spine surgery, indicating an additional year or more of specialized training.
The most effective treatment often comes from a multidisciplinary team. As highlighted by UT Health Austin's Back and Neck Pain Center, a comprehensive care team may also include:
This team-based approach ensures that you, the patient, are treated as a whole person, addressing not just the structural problem but also your functional goals and overall well-being.
The journey to recovery is a stepped process that almost always begins with the least invasive options. Up to 90% of spine issues can be successfully treated without surgery.
This is the foundation of spine care and includes:
When conservative treatments aren't enough, but surgery isn't yet warranted, advanced options can bridge the gap. A recent Newswise report highlighted one such innovation: basivertebral nerve (BVN) ablation. This minimally invasive procedure uses heat to disrupt a specific nerve responsible for chronic low back pain originating from damaged vertebral endplates, offering a new source of hope for patients with vertebrogenic pain. Other interventional treatments include radiofrequency ablation and spinal cord stimulation.
Surgery is typically reserved for cases where:
If surgery is the right path, you and your surgeon will discuss the best approach.
!A diagram comparing the smaller incision of minimally invasive spine surgery with the larger incision of traditional open surgery. Image Source: Interventional Pain Associates
The decision between MISS and open surgery is highly individualized, depending on your specific diagnosis, overall health, and your surgeon's expertise.
Navigating back and spine issues can be daunting, but understanding your condition and the available options is empowering. The key to a successful outcome is a personalized care plan developed in collaboration with a team of medical experts. Always start with a thorough diagnosis from a qualified specialist, explore all conservative treatment avenues first, and engage in open dialogue with your healthcare provider to make informed decisions that align with your health goals.