Desiccated Disc: A Comprehensive Guide to Causes, Symptoms, and Treatment

Key points
- Nucleus Pulposus: A soft, gel-like center with high water content that provides cushioning.
- Annulus Fibrosus: A tough, fibrous outer ring that protects the nucleus.
If you've received a medical report mentioning a "desiccated disc," you might be wondering what it means for your health. A desiccated disc is a common condition where the spongy cushions between your vertebrae lose moisture, leading to a variety of symptoms from mild stiffness to significant pain.
This guide synthesizes expert knowledge from top medical sources to provide a comprehensive overview of disc desiccation, covering everything from its underlying causes and symptoms to the most effective treatment strategies available today.
What is a Desiccated Disc?
Your spine is composed of 33 vertebrae stacked on top of one another. Between most of these bones are tough, spongy intervertebral discs that act as shock absorbers, allowing for flexibility and preventing the bones from grinding together.
Each disc has two main parts:
- Nucleus Pulposus: A soft, gel-like center with high water content that provides cushioning.
- Annulus Fibrosus: A tough, fibrous outer ring that protects the nucleus.
Disc desiccation is the medical term for the dehydration of these discs. As you age, the nucleus pulposus naturally loses its fluid. This causes the disc to become flatter, harder, and less effective at absorbing shock. This process is a key feature of a broader condition known as Degenerative Disc Disease (DDD).
 Image Source: Advanced Spine Center
Image Source: Advanced Spine Center
Symptoms: How Does a Desiccated Disc Feel?
While many people with disc desiccation experience no symptoms, others may face discomfort that ranges from mild to severe. The symptoms often depend on the location and severity of the condition.
Common signs of a desiccated disc include:
- Pain and Stiffness: This is the most common symptom, localized to the back or neck. Pain may worsen with certain movements like bending or twisting.
- Radiating Pain: If the flattened disc presses on a nerve, pain can travel down the arms or legs (a condition known as sciatica if it affects the sciatic nerve).
- Weakness: Muscles in the arms or legs may feel weak.
- Numbness or Tingling: A "pins-and-needles" sensation can occur in the extremities.
- Reduced Range of Motion: Difficulty moving or bending your spine as you normally would.
The location of the desiccated disc determines where symptoms are felt. Cervical (neck) desiccation can cause neck pain and headaches, while lumbar (lower back) desiccation is a common source of lower back pain.
The Stages of Disc Degeneration and Desiccation
Disc desiccation doesn't happen overnight. It's a progressive condition that experts often describe in four stages:
- Stage 1: Dysfunction and Dehydration: The disc begins to lose its ability to retain water. Small tears may form in the outer annulus fibrosus, and you might experience mild, occasional back pain.
- Stage 2: Dehydration and Prolapse: The disc continues to dry out and lose height, potentially causing it to bulge (prolapse). This can put pressure on spinal nerves, leading to more persistent pain.
- Stage 3: Stabilization and Herniation: In this advanced stage, the annulus can tear completely, allowing the nucleus to leak out—a herniated disc. The body may attempt to stabilize the area by forming bone spurs (osteophytes), which can further narrow the spinal canal.
- Stage 4: Severe Degeneration and Collapse: The disc loses a significant amount of its height and may collapse entirely. This can lead to bone-on-bone friction, causing chronic, debilitating pain and severely limited mobility.
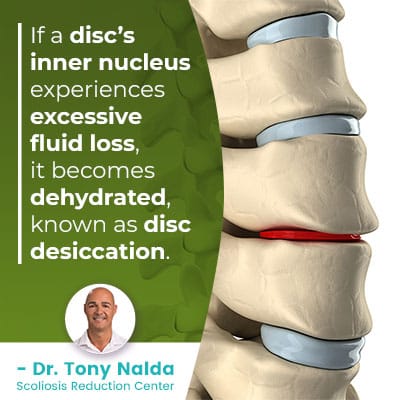 Image Source: Dr. Tony Nalda
Image Source: Dr. Tony Nalda
What Causes a Disc to Become Desiccated?
While aging is the primary driver of disc desiccation, several other factors can accelerate the process:
- Natural Aging: This is the most common cause. As we get older, our discs naturally lose water content and elasticity.
- Repetitive Strain: Jobs or activities involving heavy lifting, frequent bending, or twisting can place excessive wear and tear on the spine.
- Trauma or Injury: A sudden injury from a fall, car accident, or sports can damage a disc and trigger degeneration.
- Lifestyle Factors:
- Obesity: Excess weight puts added pressure on the spine.
- Smoking: Nicotine restricts blood flow to the discs, impairing their ability to receive nutrients and stay hydrated.
- Poor Posture: Prolonged slouching or poor ergonomics can create uneven pressure on your discs.
- Dehydration and Malnutrition: Not drinking enough water or having a poor diet can affect overall tissue health, including your discs.
- Genetics: Some people may be genetically predisposed to developing degenerative disc disease earlier in life.
Diagnosis: How Doctors Identify a Desiccated Disc
If you're experiencing persistent back or neck pain, a doctor will typically follow a standard process to diagnose the cause:
- Medical History and Physical Exam: Your doctor will ask about your symptoms, past injuries, and lifestyle. They will then perform a physical exam to test your range of motion, muscle strength, reflexes, and sensation to pinpoint the affected area.
- Imaging Tests: While a physical exam provides clues, imaging tests are needed to confirm disc desiccation.
- X-ray: Can show a narrowing of the space between vertebrae, indicating a loss of disc height.
- CT Scan: Provides a more detailed cross-sectional view of the spine.
- MRI Scan: This is the gold standard for diagnosing disc desiccation. An MRI can directly visualize the disc's water content, revealing the extent of dehydration. Healthy discs appear bright and white on an MRI, while desiccated discs look darker.
Treatment Options: Managing a Desiccated Disc
A crucial point to understand is that disc desiccation cannot be reversed. Once a disc has lost its fluid, it cannot be rehydrated. Therefore, treatment focuses on managing pain, improving function, and preventing further degeneration.
Conservative Treatments: The First Line of Defense
For most patients, non-surgical treatments are highly effective. A conservative-first approach is universally recommended.
- Physical Therapy: This is a cornerstone of treatment. A physical therapist can design a program to strengthen your core and back muscles, improve flexibility, and teach you proper posture and body mechanics.
- Pain Medication: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil) and naproxen (Aleve) can help reduce pain and inflammation. In some cases, a doctor may prescribe stronger medication or muscle relaxants.
- Lifestyle Modifications:
- Maintain a Healthy Weight: Reducing excess weight lessens the load on your spine.
- Low-Impact Exercise: Activities like walking, swimming, and yoga can strengthen muscles without jarring the spine.
- Quit Smoking: This improves blood flow and nutrient delivery to the discs.
- Stay Hydrated: Drinking plenty of water is essential for overall tissue health.
- Adjunctive Therapies: Heat and cold therapy, massage, and Transcutaneous Electrical Nerve Stimulation (TENS) units can provide additional symptom relief.
When Conservative Treatments Aren't Enough
If pain persists after several weeks or months of conservative care, your doctor may suggest more advanced options.
- Spinal Injections: Corticosteroid injections delivered into the epidural space around the spinal nerves can provide powerful, short-term relief from inflammation and pain.
- Surgical Interventions: Surgery is considered a last resort, reserved for cases with severe, debilitating pain, progressive neurological symptoms (like worsening weakness), or signs of spinal instability. Common procedures include:
- Spinal Fusion: The surgeon permanently joins two or more vertebrae to eliminate painful motion.
- Artificial Disc Replacement: The damaged disc is replaced with a prosthetic device designed to preserve motion.
- Decompression (Laminectomy or Discectomy): Bone or disc material pressing on a nerve is removed to relieve pressure.
The Role of Diet in Managing Disc Health
While diet can't reverse desiccation, an anti-inflammatory eating plan can help manage symptoms associated with degenerative disc disease.
Foods to Avoid or Limit
- Sugary and Refined Foods: Sodas, pastries, and white bread can trigger inflammation.
- Processed and Red Meats: Foods like bacon, sausage, and ham are linked to increased inflammatory markers.
- Unhealthy Fats: Limit saturated and trans fats found in fried and processed foods.
- Dehydrating Beverages: Excessive alcohol and caffeine can contribute to dehydration.
Foods to Emphasize
Focus on a diet rich in whole foods like fruits, vegetables, whole grains, and lean proteins to help manage inflammation and support overall health.
Desiccated Disc vs. Herniated Disc: What's the Difference?
It's easy to confuse these terms, but they describe different things:
- A desiccated disc is a state—the disc is dehydrated, thin, and brittle. It's a sign of degeneration.
- A herniated disc (or "slipped disc") is an event—the soft inner gel pushes through a tear in the tough outer wall.
Think of it this way: disc desiccation weakens the disc, making it more prone to tearing and herniating. A desiccated disc is a risk factor for a herniated disc.
Living with a desiccated disc can be challenging, but it is a manageable condition. By working with your healthcare provider to develop a comprehensive treatment plan that includes physical therapy, lifestyle changes, and appropriate pain management, you can significantly improve your quality of life and keep your spine as healthy as possible.
References
- Roland, J. (2017). Disc Desiccation: Symptoms, Causes, and Treatment. Healthline. https://www.healthline.com/health/disc-desiccation
- Lanman, T. (2024). Disc Desiccation: Symptoms, Causes, and Treatment. Spine.MD. https://www.spine.md/insights/articles/disc-desiccation-symptoms-causes-treatment/
- Galan, N. (2018). Disc desiccation: Symptoms, causes, and treatments. Medical News Today. https://www.medicalnewstoday.com/articles/322121
- Donnally III, C.J., & Dulebohn, S.C. (2018). Lumbar Degenerative Disk Disease. Medscape. https://emedicine.medscape.com/article/309767-overview
About the author
Samuel Jones, MD, is a board-certified orthopedic surgeon specializing in joint replacement and orthopedic trauma. He is a team physician for a professional sports team and practices at a renowned orthopedic institute in Georgia.