Diverting Loop Ileostomy: A Complete Guide to Surgery and Recovery

Key points
- The Proximal Opening: This is the "active" opening connected to the functioning part of the small intestine. It's where digestive waste (stool) exits the body into an external ostomy pouch.
- The Distal Opening: This "inactive" opening is connected to the resting part of the bowel (the colon and rectum). It only passes a small amount of mucus.
A diverting loop ileostomy is a surgical procedure that can be a critical step in treating conditions like rectal cancer, inflammatory bowel disease (IBD), and diverticulitis. While the thought of an ostomy can be daunting, understanding the procedure, its purpose, and what to expect during recovery can empower patients and their families.
This comprehensive guide synthesizes information from leading medical institutions and recent clinical research to provide a clear, in-depth look at every aspect of a diverting loop ileostomy, from the operating room to daily life.
What is a Diverting Loop Ileostomy?
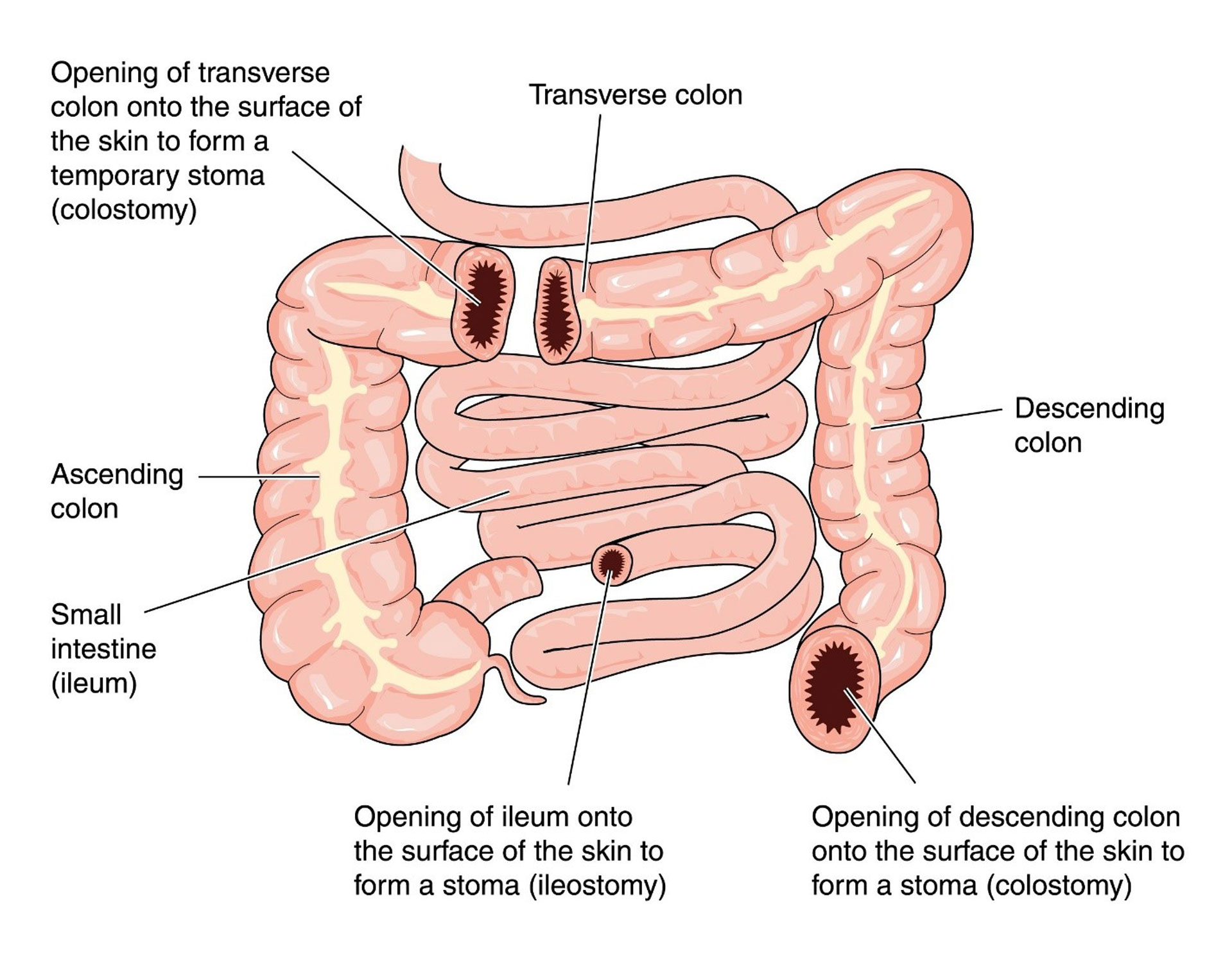
A diverting loop ileostomy is a surgical procedure that creates a temporary opening, called a stoma, on the abdomen to allow stool to exit the body, bypassing the lower parts of the digestive tract.
During the surgery, a loop of the small intestine (specifically, the final section known as the ileum) is brought through an incision in the abdominal wall. The surgeon then makes a cut in this loop and stitches it to the skin, creating a single stoma that has two distinct openings:
- The Proximal Opening: This is the "active" opening connected to the functioning part of the small intestine. It's where digestive waste (stool) exits the body into an external ostomy pouch.
- The Distal Opening: This "inactive" opening is connected to the resting part of the bowel (the colon and rectum). It only passes a small amount of mucus.
The primary goal of this procedure is to "divert" the fecal stream, giving a downstream surgical connection (anastomosis) or a diseased section of the bowel time to heal without being irritated by waste. As noted by NHS inform, this procedure is almost always intended to be temporary and is later reversed.
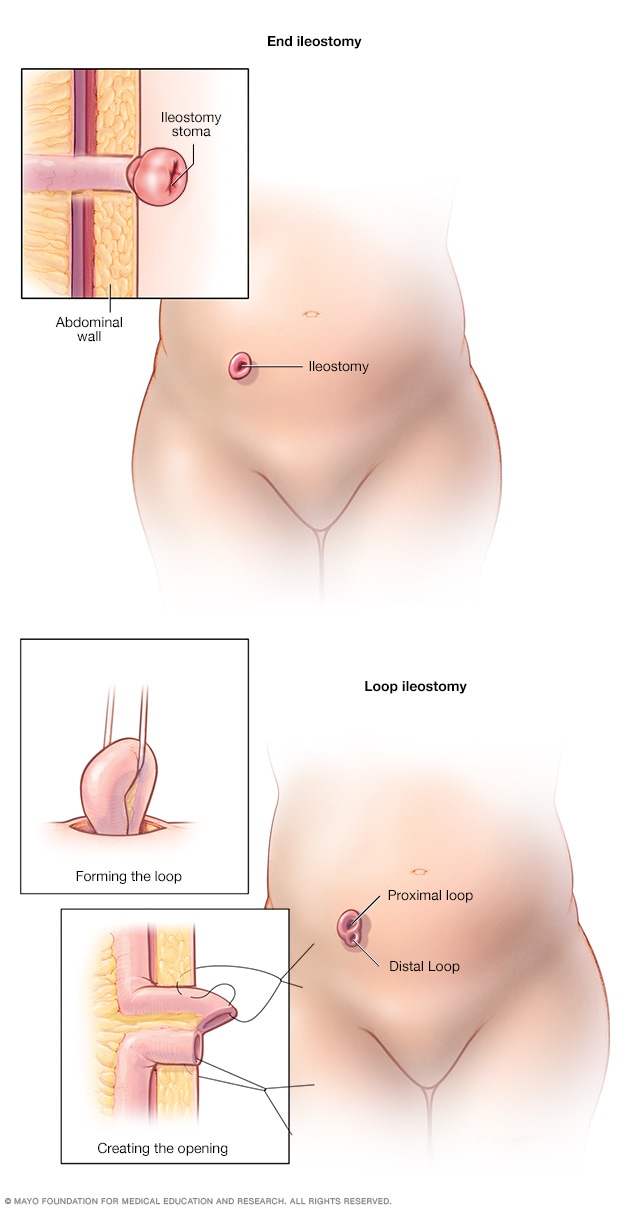 (Image Source: Mayo Clinic)
(Image Source: Mayo Clinic)
Why is a Diverting Loop Ileostomy Performed?
Surgeons recommend a diverting loop ileostomy in several clinical scenarios, primarily to protect the bowel and reduce the risk of severe complications. According to a review in the Clinics in Colon and Rectal Surgery, fecal diversion is an essential tool for managing complex colorectal conditions.
Key indications include:
- Protecting a New Surgical Anastomosis: This is the most common reason. After a surgeon removes a section of the colon or rectum (e.g., for rectal cancer) and reconnects the two ends, a temporary ileostomy protects this delicate connection from the fecal stream, reducing the consequences of a potential leak.
- Inflammatory Bowel Disease (IBD): In severe cases of Crohn's disease or ulcerative colitis, an ileostomy allows the inflamed colon and rectum to rest and heal.
- Complicated Diverticulitis: For patients with perforated diverticulitis and significant infection, a surgeon may perform a bowel resection and create a diverting ileostomy to allow the infection and inflammation to resolve before restoring bowel continuity.
- Bowel Obstruction: It can be used as a temporary measure to decompress the bowel in cases of a malignant obstruction.
- Severe Perianal Crohn's Disease: When perianal disease is severe and uncontrolled, diversion can provide symptomatic relief and allow the area to heal.
The Surgical Procedure: What to Expect
An ileostomy is considered major surgery, and preparation is key to a smooth recovery.
Preparing for Surgery
Before the operation, your surgical team will conduct a thorough assessment. A specialized Wound Ostomy Continence (WOC) nurse will meet with you to discuss life with a stoma and help mark the ideal location for it on your abdomen—a spot that is flat, visible, and away from skin folds or your beltline. You will also receive instructions on bowel preparation and dietary restrictions before surgery.
During the Surgery
The procedure is performed under general anesthesia. It can be done in two ways:
- Open Surgery: Involves one long incision down the abdomen.
- Laparoscopic (Minimally Invasive) Surgery: Uses several small incisions and a camera to perform the procedure. This approach often leads to a faster recovery.
The surgeon creates the stoma as described above, sometimes using a small plastic rod to support the loop of intestine on the outside of the abdomen for the first week.
How Long is Recovery?
As highlighted by Cleveland Clinic, recovery from an ileostomy takes about six to eight weeks. Your initial hospital stay will likely be between 3 and 10 days, where your healthcare team will monitor you closely and teach you the essentials of stoma care.
Recovery and Life with a Loop Ileostomy
Adjusting to life with a stoma takes time and patience, but most people return to their normal activities.
Caring for Your Stoma at Home
A WOC nurse is an invaluable resource during your recovery. You will learn how to manage your pouching system, which consists of a skin barrier (wafer) that sticks to your skin and a collection pouch that attaches to it.
- Emptying the Pouch: The pouch should be emptied into the toilet when it is one-third to one-half full, typically 4 to 8 times a day.
- Changing the System: The entire system (wafer and pouch) is usually changed about twice a week.
- Skin Care: Protecting the skin around your stoma (peristomal skin) is crucial. Stool from the small intestine can be very irritating to the skin, so a properly fitting wafer is essential to prevent leakage.
Diet and Nutrition
After surgery, your stool output will be liquid. Over time, it will thicken to a paste-like consistency.
- Hydration is Critical: Because stool is bypassing the colon (where water is absorbed), you are at a higher risk of dehydration. It is vital to drink 8 to 10 cups of fluid daily.
- Initial Diet: For the first few weeks, your doctor will likely recommend a low-fiber, bland diet.
- Food Blockages: Some high-fiber foods (like nuts, corn, and raw vegetables) can potentially cause a blockage. It's important to chew food thoroughly and reintroduce these items one at a time.
 (Image Source: Dr. Neeraj Singh, MD, FACS, FASCRS)
(Image Source: Dr. Neeraj Singh, MD, FACS, FASCRS)
Daily Life and Activities
With proper care, an ileostomy shouldn't limit you.
- Showering and Swimming: You can shower and swim with or without your pouch on. Water will not harm the stoma.
- Clothing: Most clothing will fit comfortably over your ostomy. Many people prefer avoiding tight waistbands directly over the stoma.
- Exercise and Travel: Once you have recovered, you can return to most physical activities. With some planning, travel is entirely possible—just be sure to pack extra supplies.
- Intimacy: Open communication with your partner is key. Smaller pouches or pouch covers can help with confidence.
Potential Risks and Complications
While generally safe, a loop ileostomy has potential complications. The most common issues include:
- Dehydration and Electrolyte Imbalance: Due to high liquid output, this is a primary concern and a frequent reason for hospital readmission.
- Skin Irritation: Leakage of stool onto the skin can cause painful rashes and breakdown.
- Stoma Prolapse or Retraction: The stoma may protrude further out or sink below the skin level.
- Parastomal Hernia: The abdominal muscles around the stoma may weaken, causing a bulge.
- Food Blockage: As mentioned, certain foods can obstruct the stoma, causing pain, cramping, and a stop in output.
Loop Ileostomy Reversal (Closure)
The good news is that a diverting loop ileostomy is designed to be temporary. The reversal surgery is a less invasive procedure where the surgeon reconnects the loop of the ileum and closes the stoma site on the abdomen.
When is Reversal Performed? The Timing Debate
The traditional timeline for reversal is around 3 to 6 months after the initial surgery. However, recent research, including a 2025 study in Surgery, notes that the actual time to reversal is often longer, with a median of 5.5 months for rectal cancer patients. Delays can be caused by the need for adjuvant chemotherapy, postoperative complications, or scheduling issues.
There's an ongoing clinical debate about the optimal timing:
- Early Reversal (within 2 months): May reduce the time a patient lives with a stoma and its associated complications, but some studies suggest a slightly higher risk of reversal-related complications like bowel obstruction.
- Delayed Reversal (after 5-6 months): Waiting too long may increase the risk of digestive issues like diarrhea and incontinence after reversal.
The decision is highly individualized and made in consultation with your surgeon.
Risks of Reversal Surgery
While safer than the initial operation, reversal surgery carries its own risks:
- Anastomotic Leak: The reconnected bowel may leak.
- Small Bowel Obstruction: Scar tissue can cause a blockage.
- Incisional Hernia: A hernia can develop at the closed stoma site.
- Infection: As with any surgery, there is a risk of infection.
Diverting Loop Ileostomy vs. Other Stomas
It's helpful to understand how a loop ileostomy compares to other types of stomas.
Loop Ileostomy vs. End Ileostomy
| Feature | Diverting Loop Ileostomy | End Ileostomy |
|---|---|---|
| Duration | Usually temporary | Usually permanent |
| Structure | A loop of intestine creates one stoma with two openings | The end of the intestine creates one stoma with a single opening |
| Purpose | To divert stool to protect a healing surgical site | To permanently divert stool when the large intestine is removed |
| Reversal | Simpler reversal procedure | Reversal is more complex and often not possible |
Loop Ileostomy vs. Loop Colostomy
The choice between an ileostomy (small intestine) and a colostomy (large intestine) for temporary diversion is a topic of much clinical research.
- Ileostomy Output: Liquid to paste-like, high volume.
- Colostomy Output: Thicker to more formed, lower volume.
A meta-analysis cited by the National Institutes of Health (NIH) found that loop ileostomies are generally preferred because they are associated with lower rates of stoma prolapse and sepsis. However, loop ileostomies carry a significantly higher risk of dehydration and acute kidney injury due to high output. A loop colostomy may be chosen for patients with pre-existing kidney problems or if the diversion is expected to be long-term.
The Clinical Debate: When is Diversion Necessary?
While a diverting ileostomy can be lifesaving, it comes with its own set of complications and a significant impact on quality of life. This has led to a clinical debate on whether it should be used routinely in certain procedures (like low rectal cancer surgery) or only selectively for high-risk patients.
The current consensus leans towards selective use. Factors that place a patient at high risk for an anastomotic leak, and therefore make them a strong candidate for a diverting ileostomy, include:
- A very low anastomosis (close to the anus)
- Male gender
- Malnutrition
- Pre-operative radiation
- A technically difficult surgery
The decision for fecal diversion should always be a shared one between the surgeon and the patient after a thorough discussion of the risks and benefits.
References
- Mayo Clinic. (2025). Ileostomy. https://www.mayoclinic.org/tests-procedures/ileostomy/about/pac-20582350
- Plasencia, A., et al. (2019). Diverting Ostomy: For Whom, When, What, Where, and Why. Clinics in Colon and Rectal Surgery, 32(3), 156–162. https://pmc.ncbi.nlm.nih.gov/articles/PMC6500738/
- Withe, M. (2024). Loop ileostomy: What to expect, risks, and reversal. Medical News Today. https://www.medicalnewstoday.com/articles/loop-ileostomy
- Cleveland Clinic. (2023). Ileostomy: What Is It, Types, Bags, Surgery & Complications. https://my.clevelandclinic.org/health/procedures/21726-ileostomy
- Boyer, M.E., et al. (2025). Assessing the pathway and timing for ileostomy reversal in rectal cancer: A retrospective cohort study. Surgery. https://www.sciencedirect.com/science/article/abs/pii/S0039606025003599

About the author
Fatima Al-Jamil, MD, MPH, is board-certified in gastroenterology and hepatology. She is an Assistant Professor of Medicine at a university in Michigan, with a clinical focus on inflammatory bowel disease (IBD) and motility disorders.