Understanding Your Risk of Cervical Cancer After a LEEP Procedure

Key points
- Negative Margins: This is the ideal outcome. It means there are no abnormal cells at the edges of the removed tissue, suggesting the entire lesion was successfully excised.
- Positive Margins (or Involved Margins): This means abnormal cells were found at the edge of the tissue sample. It indicates that some precancerous cells may have been left behind on the cervix.
If you've been told you need a Loop Electrosurgical Excision Procedure (LEEP), it's natural to have questions and concerns, especially about what comes next. A LEEP is a common and highly effective procedure used to remove abnormal, precancerous cells from the cervix. While its primary goal is to prevent cervical cancer, many wonder about the long-term risk.
This comprehensive guide synthesizes data from clinical studies and medical experts to provide a clear picture of the chances of developing cervical cancer after a LEEP, the factors that influence your risk, and the critical importance of follow-up care.
The LEEP Procedure: A Powerful Tool for Cervical Cancer Prevention
A LEEP is performed after abnormal cells are detected during a Pap smear or colposcopy. It uses a thin, low-voltage electrified wire loop to precisely cut away the affected tissue from the cervix. This tissue is then sent to a lab for further analysis.
The procedure serves two purposes:
- Diagnostic: It confirms the severity of the abnormal cells (cervical intraepithelial neoplasia, or CIN).
- Therapeutic: It removes the precancerous cells, which in many cases is the only treatment needed.
LEEP is considered a cornerstone of cervical cancer prevention, with a success rate of over 90% in removing abnormal cells and preventing progression to cancer.
Illustration of the LEEP procedure. Source: Cleveland Clinic.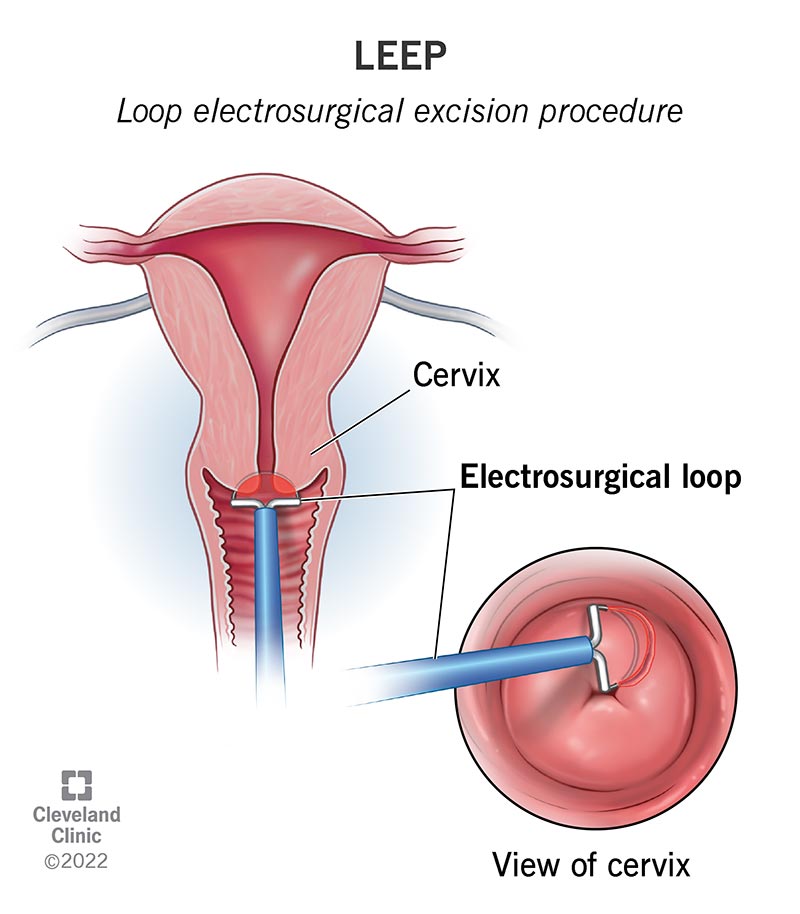
What Are the Chances of Cervical Cancer After LEEP? The Statistics
First, the reassuring news: the risk of developing invasive cervical cancer after a successful LEEP is very low. Medical experts estimate this risk to be around 1-2%.
It's more common for precancerous cells (CIN) to recur. This is not cancer, but it requires monitoring and sometimes further treatment.
| Outcome After LEEP | Estimated Risk | What It Means |
|---|---|---|
| Recurrence of Precancerous Cells (CIN) | 5% - 10% | Abnormal cells have returned, requiring diligent follow-up and potentially more treatment. |
| Development of Invasive Cervical Cancer | 1% - 2% | The condition has progressed to cancer, which is a rare outcome after LEEP. |
These statistics underscore that while LEEP is highly effective, it is not a 100% cure. Your individual risk depends on several key factors identified during and after the procedure.
Key Factors That Influence Your Post-LEEP Risk
Understanding what influences the risk of recurrence can empower you to take a proactive role in your health. Research consistently points to two critical factors: surgical margins and HPV status.
Surgical Margin Status: Was It All Removed?
When the tissue is removed during a LEEP, a pathologist examines the edges, or "margins," under a microscope.
- Negative Margins: This is the ideal outcome. It means there are no abnormal cells at the edges of the removed tissue, suggesting the entire lesion was successfully excised.
- Positive Margins (or Involved Margins): This means abnormal cells were found at the edge of the tissue sample. It indicates that some precancerous cells may have been left behind on the cervix.
Positive margins are a significant predictor of recurrence. One large-scale study published in the Journal of Cancer Research and Clinical Oncology found that patients with positive margins had a 29.8% recurrence rate, compared to just 2.8% for those with negative margins.
HPV Persistence: The Most Critical Factor
The LEEP procedure removes the cervical cells that have been damaged by the Human Papillomavirus (HPV), but it does not eliminate the virus from your body. Your immune system is responsible for clearing the underlying HPV infection.
Persistent high-risk HPV (hr-HPV) infection is the single most important risk factor for the recurrence of CIN after LEEP.
A 2024 meta-analysis provided compelling evidence:
- With negative margins and no detectable HPV after LEEP, the recurrence rate of CIN was a mere 0.5%.
- With negative margins but persistent HPV infection, the recurrence rate surged to 18%.
This highlights why follow-up HPV testing is just as important, if not more so, than the margin status.
Other Contributing Risk Factors
Several other factors can play a role in your risk profile:
- High-Grade Lesion (CIN 3): Patients with more advanced precancerous changes (CIN 3) have a higher risk of recurrence than those with CIN 2.
- Age: Some studies suggest women over 40 may have a higher risk of recurrence.
- Smoking: Smoking weakens the immune system's ability to fight HPV and is a known independent risk factor for both cervical cancer and post-LEEP recurrence.
- Weakened Immune System: Conditions like HIV or taking immunosuppressant drugs can make it harder for the body to clear HPV, increasing recurrence risk.
Understanding risk factors is key to managing health after a LEEP. Source: Thomson Medical.
Life After LEEP: Recovery, Follow-Up, and Long-Term Health
Your care doesn't end when the procedure is over. The post-LEEP period is crucial for healing and long-term prevention.
Navigating the Recovery Period
Recovery typically takes about four weeks. During this time, you can expect:
- Mild cramping, similar to a menstrual period.
- Watery vaginal discharge, which may be pinkish or have a slight odor.
- A dark, coffee-ground-like discharge, which is from the medicated paste used to control bleeding.
To ensure proper healing, your doctor will advise you to avoid the following for at least four weeks:
- Vaginal intercourse
- Using tampons or menstrual cups (use pads instead)
- Douching
- Heavy lifting or strenuous exercise
- Bathing or swimming (showers are fine)
Contact your doctor if you experience severe abdominal pain, heavy bleeding (soaking more than one pad an hour), fever, or foul-smelling discharge, as these could be signs of an infection or complication.
The Importance of Long-Term Surveillance
A LEEP is not a "one-and-done" treatment. Consistent, long-term follow-up is non-negotiable and the most important step you can take to protect your health.
Current guidelines, such as those from the American Society for Colposcopy and Cervical Pathology (ASCCP), recommend co-testing (a Pap test and an HPV test) 6 months after the LEEP procedure.
- If these tests are negative, you will likely continue with regular screenings.
- If either test is positive, your doctor may recommend a colposcopy to investigate further.
This surveillance schedule is crucial for catching any persistent or recurrent disease early, when it is most treatable.
What Happens if Abnormal Cells Return?
If follow-up testing reveals that high-grade dysplasia has persisted or recurred, your doctor will discuss the next steps. This is known as an escalation of care. The options depend on the severity of the cells, your age, and your desire for future pregnancies.
- Repeat LEEP: For many, especially those who wish to preserve fertility, a second LEEP procedure can be performed to remove the remaining abnormal tissue.
- Hysterectomy: For women who have completed childbearing or when a repeat excision is not a suitable option, a hysterectomy (surgical removal of the uterus and cervix) is a definitive treatment that eliminates the risk of cervical cancer.
Conclusion: A Proactive Approach to Your Cervical Health
Receiving a diagnosis of cervical dysplasia and undergoing a LEEP can be a stressful experience, but it's important to view it as a proactive and highly effective step in preventing cancer. The chance of developing cervical cancer after a LEEP is very low.
Your long-term health depends on a partnership between you and your healthcare provider. By understanding the key risk factors like HPV persistence and adhering strictly to your recommended follow-up schedule, you can significantly minimize your risk and ensure any potential issues are addressed immediately.
References
- Medical News Today. (2023). Odds of cervical cancer after LEEP: Effectiveness and more. Retrieved from https://www.medicalnewstoday.com/articles/chances-of-cervical-cancer-after-leep
- Healthline. (2024). Chances of Cervical Cancer After a LEEP Procedure. Retrieved from https://www.healthline.com/health/cervical-cancer/chances-of-cervical-cancer-after-leep
- Cleveland Clinic. (2022). Loop Electrosurgical Excision Procedure (LEEP). Retrieved from https://my.clevelandclinic.org/health/treatments/4711-loop-electrosurgical-excision-procedure-leep
- Ding, T., et al. (2022). Risk factors analysis of recurrent disease after treatment with a loop electrosurgical excision procedure in patients with cervical intraepithelial neoplasia 2–3: a retrospective study of 4369 patients. Journal of Cancer Research and Clinical Oncology. Retrieved from https://pmc.ncbi.nlm.nih.gov/articles/PMC10087663/
- Bogani, G., et al. (2020). Recurrence rate after loop electrosurgical excision procedure (LEEP) and laser Conization: A 5-year follow-up study. Gynecologic Oncology. Retrieved from https://www.sciencedirect.com/science/article/abs/pii/S0090825820338269
- Johns Hopkins Medicine. Fertility and Pregnancy After a LEEP. Retrieved from https://www.hopkinsmedicine.org/health/wellness-and-prevention/fertility-and-pregnancy-after-a-leep

About the author
Sofia Rossi, MD, is a board-certified obstetrician-gynecologist with over 15 years of experience in high-risk pregnancies and reproductive health. She is a clinical professor at a top New York medical school and an attending physician at a university hospital.